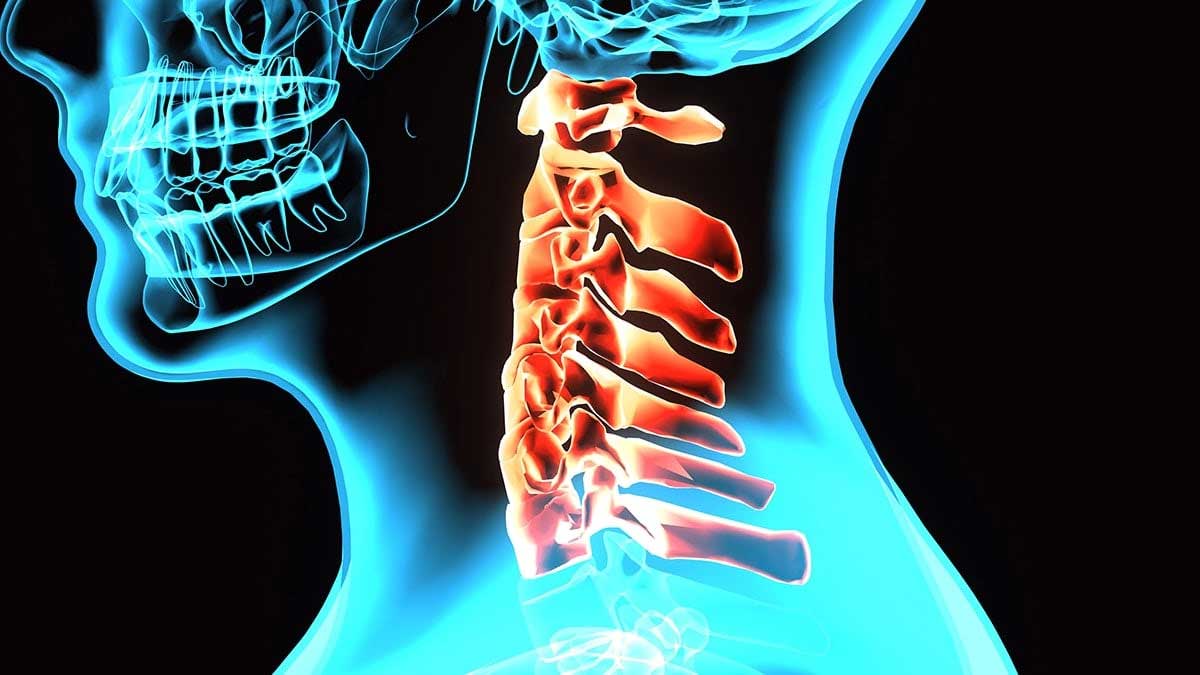
A broken neck, medically referred to as a cervical spine fracture, is one of the most serious traumatic injuries a person can experience. The cervical spine consists of seven vertebrae (C1–C7) that support the head, protect the spinal cord, and allow for a wide range of motion. When any of these vertebrae fracture or become unstable, the consequences can be life-altering. Doctors emphasize that the true danger often lies not only in the fracture itself but in the Complications of a broken neck, which may affect nearly every system in the body.
Understanding the Complications of a broken neck is critical for patients, caregivers, and healthcare providers alike. These complications can develop immediately after the injury or appear gradually over weeks and months. Early recognition, prompt medical care, and comprehensive rehabilitation are essential to reducing long-term disability and improving survival rates.
Understanding Cervical Spine Fractures
A broken neck typically results from high-impact trauma such as car accidents, falls from height, sports injuries, or violent incidents. In older adults, even minor falls can cause fractures due to osteoporosis. The cervical spine houses and protects the upper portion of the spinal cord, which transmits signals between the brain and the rest of the body. Damage in this region can disrupt breathing, movement, sensation, and organ function.
The severity of injury varies widely. Some fractures are stable and may heal with immobilization using a cervical collar or brace. Others are unstable and require surgical intervention to prevent spinal cord damage. Doctors categorize injuries based on their location, mechanism, and associated neurological involvement. When the spinal cord is compressed or severed, the risk of severe Spinal cord injury complications increases dramatically.
Immediate Neurological Complications

One of the most feared Complications of a broken neck is spinal cord damage. The cervical spinal cord controls movement and sensation in the arms, trunk, and legs, as well as diaphragm function. Injury at higher cervical levels (C1–C4) may impair breathing, requiring mechanical ventilation.
Paralysis
Depending on the level and extent of spinal cord damage, patients may develop:
Quadriplegia (tetraplegia): Paralysis of all four limbs.
Partial paralysis: Weakness or loss of function in specific muscle groups.
These conditions are among the most devastating Spinal cord injury complications, often requiring lifelong assistance and adaptive equipment.
Loss of Sensation
In addition to motor deficits, patients may lose sensation below the level of injury. This includes reduced ability to feel pain, temperature, or touch, increasing the risk of burns, pressure sores, and unnoticed injuries.
Respiratory Complications
Respiratory failure is a common and life-threatening Complications of a broken neck, especially when the injury affects the upper cervical spine. The diaphragm, the primary muscle responsible for breathing, is controlled by the phrenic nerve originating from C3–C5.
Breathing Difficulties
Patients may experience:
- Shallow breathing
- Reduced lung capacity
- Increased susceptibility to pneumonia
Ventilator dependence may be temporary or permanent. Doctors closely monitor oxygen levels, lung function, and signs of infection during the acute phase of care.
Cardiovascular and Blood Pressure Instability
A broken neck can disrupt the autonomic nervous system, which regulates heart rate and blood pressure. This may lead to:
- Bradycardia (slow heart rate)
- Hypotension (low blood pressure)
- Autonomic dysreflexia in chronic cases
Autonomic dysreflexia is a serious condition characterized by sudden high blood pressure, headaches, and sweating, typically occurring in patients with spinal cord injuries above T6. Though more common in lower cervical injuries, it remains an important concern in the spectrum of Spinal cord injury complications.
Chronic Pain and Musculoskeletal Issues
Even when paralysis does not occur, chronic pain is a frequent Complications of a broken neck. Pain may originate from:
- Nerve compression
- Muscle spasm
- Joint instability
- Post-surgical changes
Neck stiffness and limited range of motion can persist long after the fracture heals. Some patients also develop secondary problems in adjacent areas due to altered posture and biomechanics.
For example, patients immobilized for long periods may complain about shoulder discomfort. In clinical practice, doctors sometimes evaluate overlapping symptoms by reviewing resources such as The most important causes of shoulder pain to distinguish between referred pain from cervical injury and independent shoulder pathology.
Psychological and Emotional Consequences
The psychological burden following a broken neck is significant. Depression, anxiety, and post-traumatic stress disorder (PTSD) are common, especially in patients facing permanent disability.
Adjustment to Disability
Adapting to a new lifestyle that may include mobility aids, caregivers, and medical devices can be overwhelming. Emotional distress may worsen physical recovery, making psychological support an essential component of treatment.
Doctors stress that mental health care is not optional but a critical aspect of managing the broader Complications of a broken neck. Counseling, peer support groups, and psychiatric treatment can improve long-term outcomes.
Secondary Complications from Immobility
Prolonged immobility after cervical spine fractures increases the risk of several additional health problems:
Pressure Ulcers
Patients with limited mobility are prone to pressure sores, especially if sensation is reduced. These wounds can become infected and difficult to treat.
Deep Vein Thrombosis (DVT)
Reduced movement in the legs may lead to blood clot formation. Pulmonary embolism, a potentially fatal condition, can occur if a clot travels to the lungs.
Muscle Atrophy
Extended immobilization causes muscle wasting, joint stiffness, and reduced endurance. Rehabilitation aims to counteract these effects through physical therapy and gradual strengthening exercises.
It is important to note that rehabilitation programs must be carefully designed. Improper training can worsen the patient’s condition. Healthcare providers often caution against activities similar to Wrong exercise injuries for legs and back, emphasizing that supervised therapy is essential to prevent additional harm.
Digestive and Bladder Dysfunction

The spinal cord also regulates bladder and bowel function. Cervical injuries can disrupt these processes, leading to:
- Urinary retention
- Incontinence
- Constipation
- Increased risk of urinary tract infections
Long-term catheter use may be required in severe cases. Doctors consider these issues among the most challenging Spinal cord injury complications, as they significantly affect quality of life and independence.
Rehabilitation and Long-Term Management
Recovery from a broken neck does not end after surgery or immobilization. Comprehensive rehabilitation includes:
- Physical therapy
- Occupational therapy
- Respiratory therapy
- Psychological support
Therapists may incorporate gentle mobility techniques. However, they strictly follow evidence-based protocols and avoid unsafe practices. For instance, while patients may inquire about massage therapy, clinicians emphasize the importance of Correct methods of neck massage without injury to prevent re-traumatizing the cervical spine.
Additionally, strengthening surrounding muscle groups can improve spinal stability. In cases where lumbar strain develops due to compensatory posture, therapists might recommend safe alternatives aligned with guidelines similar to best exercises for lumbar disc, ensuring that spinal alignment is preserved.
Surgical Complications
Surgery is often necessary for unstable fractures. Procedures may involve spinal fusion, instrumentation with plates and screws, or decompression of the spinal cord.
Infection
Postoperative infection can occur at the incision site or deeper within the spine. Early signs include redness, swelling, fever, and increased pain.
Hardware Failure
Metal implants may loosen or break, especially if bone healing is incomplete. This may require revision surgery.
Nerve Damage
Although rare, surgical manipulation can cause additional nerve injury. Surgeons take meticulous precautions to minimize this risk.
These surgical risks are considered part of the broader Complications of a broken neck, and patients are informed about them before consenting to procedures.
Impact on Daily Living

The long-term consequences of cervical spine fractures extend beyond physical symptoms. Many patients face:
- Loss of employment
- Financial strain
- Dependence on caregivers
- Reduced social interaction
Family members also experience emotional and practical challenges. Coordinated care involving social workers, rehabilitation specialists, and medical teams helps address these multifaceted concerns.
Interestingly, doctors sometimes draw comparisons between recovery protocols for different fractures. For example, while discussing spinal injury rehabilitation, they may reference principles similar to important care needed after a broken leg to highlight the importance of gradual mobilization, nutritional support, and prevention of complications.
Risk Factors for Severe Outcomes
Not all neck fractures lead to catastrophic outcomes. Doctors identify several factors that increase the likelihood of severe Complications of a broken neck:
- High-energy trauma
- Delayed medical treatment
- Advanced age
- Pre-existing spinal conditions
- Osteoporosis
Rapid emergency response and early immobilization significantly reduce the risk of worsening spinal cord damage.
Preventing Secondary Injury
Prevention plays a crucial role in minimizing Complications of a broken neck. Emergency responders are trained to stabilize the cervical spine at the scene of an accident. Improper handling can convert a stable fracture into a catastrophic spinal cord injury.
In hospital settings, multidisciplinary teams coordinate to prevent secondary complications such as infections, blood clots, and respiratory failure. Strict protocols guide patient repositioning, respiratory exercises, and medication management.
Prognosis and Recovery Outlook
The prognosis after a broken neck varies widely. Patients without spinal cord involvement may recover fully with appropriate treatment. However, those with significant neurological damage may experience permanent deficits.
Advancements in surgical techniques, critical care, and rehabilitation have improved survival rates and functional outcomes. Experimental treatments, including stem cell research and neuroregenerative therapies, offer hope for the future, though they remain under investigation.
Doctors emphasize that early intervention, patient education, and adherence to rehabilitation plans are key to improving long-term outcomes and reducing the risk of Spinal cord injury complications.
The Importance of Long-Term Follow-Up
Even years after the initial injury, patients remain at risk for delayed issues such as:
- Chronic neuropathic pain
- Degenerative changes above or below the fusion site
- Recurrent infections
- Psychological challenges
Regular medical follow-up ensures that emerging problems are identified and treated promptly. Long-term care plans often involve neurologists, orthopedic surgeons, physiatrists, and mental health professionals.
Conclusion
A broken neck is far more than a simple fracture. It is a complex medical emergency with the potential to affect every aspect of a person’s life. The Complications of a broken neck range from immediate life-threatening conditions like respiratory failure to long-term issues such as paralysis, chronic pain, and psychological distress.
Understanding the full scope of Complications of a broken neck enables patients and families to make informed decisions about treatment and rehabilitation. With early medical intervention, structured rehabilitation, and comprehensive long-term care, many complications can be managed or minimized.
While the path to recovery may be long and challenging, modern medicine offers hope through advanced surgical techniques, multidisciplinary rehabilitation, and ongoing research. Ultimately, awareness, prevention, and proactive management remain the strongest tools in reducing the burden of Complications of a broken neck and improving quality of life for those affected.







